- 1Department of Endocrinology and Metabolism, Geriatric Hospital of Nanjing Medical University, Nanjing, China
- 2Department of Public Health, Nanjing Maternity and Child Health Care Hospital, Women’s Hospital of Nanjing Medical University, Nanjing, China
Aims: To explore the clinical characteristics among elderly (aged ≥60 years) patients with type 2 diabetes (T2DM) of different durations.
Methods: Clinical characteristics were investigated in 3840 elderly T2DM patients according to their different durations of diabetes (< 1 year, 1~5 years, 5~10 years, and ≥ 10 years). Kruskal-Wallis and Dunn tests were used to assess the differences among groups for continuous variables. The chi-square and post hoc tests were carried out for dichotomous variables. The logistic regression was adopted to investigate the relationships between various durations of diabetes and the control rates of achieving the control targets for T2DM as well as diabetic vascular complications.
Results: There were 972, 896, 875 and 1097 patients with a duration of diabetes of <1, 1~5, 5~10 and ≥10 years, respectively. In logistic regression models adjusted for age, sex, education, BMI, smoking and family history of diabetes, elderly T2DM patients with a duration of diabetes of ≥10 years were more likely to reach the comprehensive control targets for TC (ORTC = 1.36, 95% CI =1.14-1.63), LDL-C (ORLDL-C = 1.39, 95% CI =1.17-1.66), TG (ORTG = 1.76, 95% CI =1.46-2.12) and BMI (ORBMI = 1.82, 95% CI =1.52-2.18). Elderly T2DM patients with a duration of diabetes of 1~5 years were more likely to achieve the HbA1c control target (ORHbA1c = 1.92, 95% CI = 1.59-2.31) than elderly T2DM patients with a duration of diabetes of <1 year. Furthermore, in elderly T2DM patients with a duration of diabetes of 5~10 years or ≥ 10 years, the duration of diabetes was positively associated with diabetic macrovascular complications (coronary heart disease and peripheral artery disease). In elderly T2DM patients with a duration of diabetes of over 10 years, the duration of diabetes was associated with diabetes kidney disease (all P < 0.05).
Conclusions: It is worth noting that the clinical characteristics of elderly patients with type 2 diabetes in different durations of diabetes are different.
Introduction
Diabetes is a metabolic disease characterized by chronic hyperglycaemia that is prevalent in China and globally. The global diabetes map (Ninth Edition), released by the International Diabetes Federation, shows that the number of patients with diabetes worldwide is 463 million currently and will increase to 700 million by 2045. China has the largest number of patients with diabetes and the largest elderly diabetic population (1). The ageing population and increasing elderly diabetic population have placed a heavy burden on health systems and the social economy (2, 3).
Type 2 diabetes mellitus (T2DM) is the most common clinical type of diabetes, accounting for nearly 90% of all diabetic cases (4). In addition to the damage resulting from hyperglycaemia and diabetic macrovascular and microvascular complications, the harmful effects of T2DM are mainly caused by comorbidities such as hypertension, dyslipidaemia, overweight and obesity. These conditions could result in a low quality of life and shortened life expectancy (5).
According to the guidelines of prevention and treatment for Chinese T2DM (2020 edition), in addition to achieving glycosylated haemoglobin (HbA1c) < 7% and maintaining glucose levels within the target range, the comprehensive management of T2DM also includes the control of other risk factors, such as hypertension, dyslipidaemia, overweight and obesity (6). Good T2DM comprehensive management can reduce the incidence of diabetic complications and comorbidities (7). Our previous research found that elderly patients (aged ≥ 80 years) with T2DM were more likely to achieve HbA1c and lipid profile targets than younger patients (aged < 60 years) (8). However, the impact of diabetes duration on the comprehensive management of T2DM remains to be explored. Furthermore, since age and diabetic duration are both major risk factors for diabetic complications (9), it is crucial to understand the differences in clinical characteristics in T2DM patients with different durations of diabetes, especially in elderly individuals.
In the present cross-sectional study, we aimed to explore the relationships between diabetes duration and the comprehensive management of T2DM as well as diabetic vascular complications in Chinese elderly patients with T2DM.
Methods
Study population
A population of 5516 elderly patients with T2DM (aged ≥ 60 years) visited the Geriatric Hospital of Nanjing Medical University in Nanjing, China, between Jan 2013 and Dec 2020. The diagnosis of T2DM was based on the diagnostic criteria of the World Health Organization in 1999 (10). After excluding those who had a history of type 1 diabetes, latent autoimmune diabetes in adults (LADA), or secondary diabetes or those who had any missing data for key variables including blood pressure, HbA1c, total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) triglyceride (TG) and body mass index (BMI), a total of 3840 elderly patients with T2DM were finally eligible for analysis. Patients were divided into four groups according to diabetic duration: < 1 year (Group 1), 1~5 years (Group 2), 5~10 years (Group 3), and ≥ 10 years (Group 4). The Ethics Committee of the Geriatric Hospital of Nanjing Medical University approved the study protocol. Each patient signed written informed consent.
Data sources
The clinical data of all elderly patients with T2DM were collected from the electronic medical record system. These information included diabetes duration, age, sex, education level, smoking status, family history of diabetes, systolic pressure (SBP), diastolic pressure (DBP), BMI, HbA1c, TG, TC, LDLC, HDL-C, therapeutic regimens, such as diabetes treatment (diet and exercise alone and anti-hyperglycaemic agents), and antihypertensive agents. Education level was defined as ≥ 9 years or < 9 years. Smoking status was divided into two groups, current smoking and non-current smoking. BMI was calculated as weight (kg)/height (m)2. Overnight fasting venous blood samples were obtained to measure HbA1c. All blood samples were measured at the laboratory of the Geriatric Hospital of Nanjing Medical University.
The data of macrovascular and microvascular complications of diabetes were also collected based on the available information. The diagnosis of coronary heart disease (CHD) was based on a history of angina pectoris, myocardial infarction, percutaneous coronary intervention or coronary artery bypass. The diagnosis of peripheral artery disease (PAD) was based on an ankle-brachial pressure index (ABI) < 0.9. The estimated glomerular filtration rate (eGFR) was calculated by the CKD-EPI formula (11), and the diagnosis of diabetes kidney disease (DKD) was based on the KDIGO clinical practice guidelines (12, 13). Albuminuria was defined as a urine albumin/creatinine ratio (ACR) > 30 mg/gCr. Patients with eGFR < 60 ml·min-1 ·1.73m2 or albuminuria were defined as having DKD.
Comprehensive control targets for T2DM
According to the guidelines for Chinese T2DM (2020 edition) (6), the T2DM control targets of comprehensive management include BP<130/80 mmHg, HbA1c < 7%, TC < 4. 5 mmol/L, LDL-C < 2. 6 mmol/L, HDL-C >1.0 mmol/L (males) or >1.3 mmol/L(females), TG< 1. 7 mmol/L, and BMI < 24.0 kg/m2.
Statistical analysis
Our clinical characteristics were non-normally distributed, descriptive information was presented as median (interquartile range [IQR]) for continuous variables or numbers and percentages for categorical variables. For continuous variables, Kruskal-Wallis and post hoc multiple comparison Dunn’s tests were used to test for the differences (R package FSA). For categorical variables, χ2 tests and post hoc tests were carried out to examine the significant differences (R package companion). Logistic regression analysis was used to calculate the odds ratios (ORs) and 95% confidence intervals (95% CIs) for the T2DM achieved control targets or the associations of different diabetic duration groups with the risks of diabetic macrovascular and microvascular complications. The unadjusted ORs and 95% CIs were calculated in Model 1. Two other models were progressively adjusted for age, sex, education, BMI (Model 2), smoking and family history of diabetes (Model 3). Patients with a diabetes duration < 1 year were the reference group. P values for trend were calculated by modeling ordinal categories as continuous variables. A two-tailed threshold of P < 0.05 was considered statistically significant. Missing data was presented as not available and were not taken into consideration during analysis. The statistics were calculated using R statistical software version 4.1.0.
Results
Baseline characteristics of elderly patients with T2DM among different diabetic duration groups
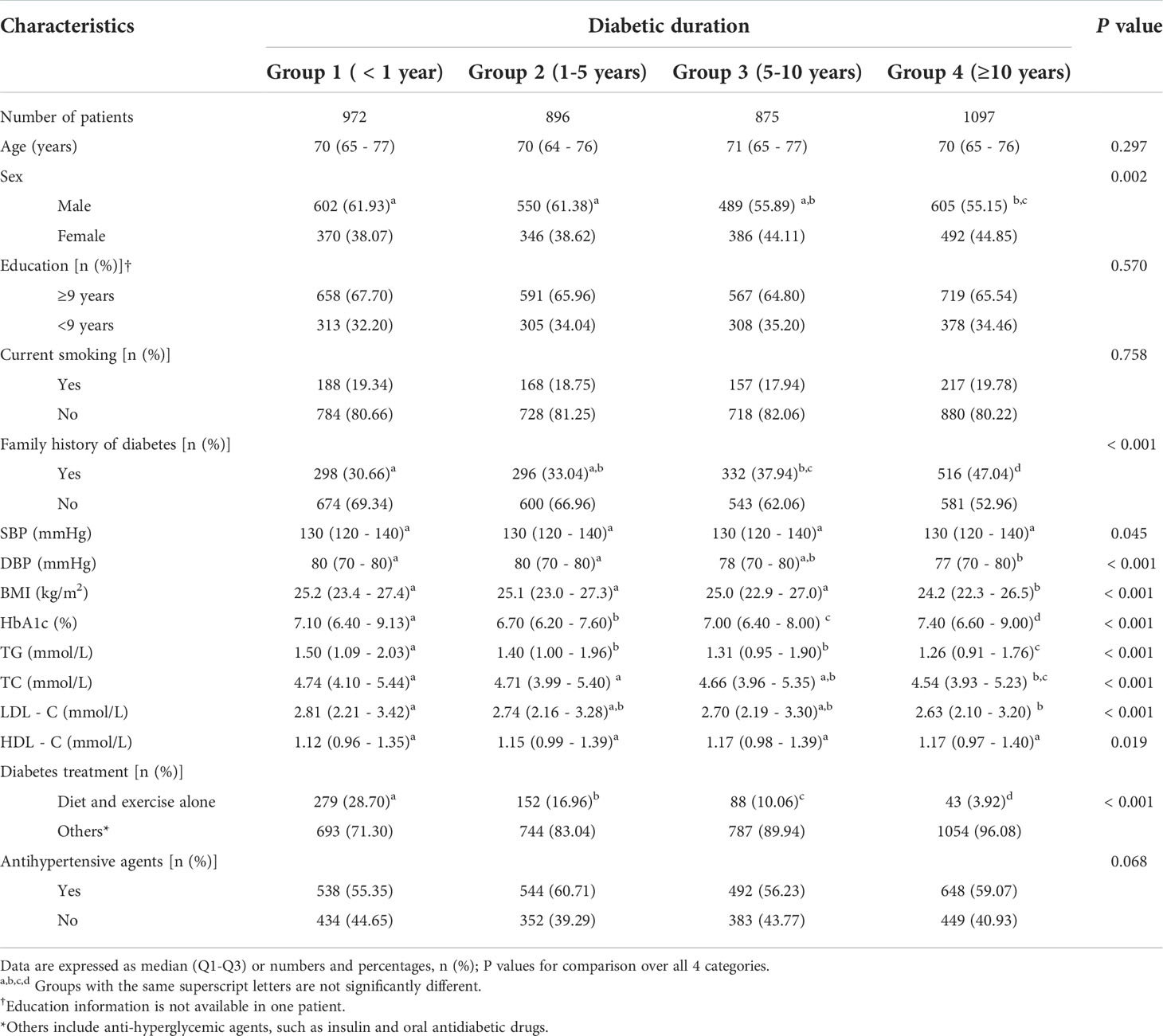
The characteristics of elderly patients with T2DM according to different diabetic duration groups are described in ###$###
Table 1. A total of 3840 elderly patients with T2DM were classified as group 1 (n = 972), group 2 (n = 896), group 3 (n = 875) and group 4 (n = 1097). Between the four groups, there were no significant differences in age, SBP, the proportion of higher education, current smoking and patients who used antihypertensive agents (all P > 0.05). In group 4, compared with groups 1 and 2, there was a significantly decreased percentage of male (Pgroup 4 vsgroup 1 = 0.013, Pgroup 4 vs group 2 = 0.035) and lower levels of DBP (Pgroup 4 vsgroup 1 < 0.001, Pgroup 4 vs group 2 = 0.014), BMI (Pgroup 4 vsgroup 1 <0.001, Pgroup 4 vs group 2 < 0.001), TG (Pgroup 4 vsgroup 1 < 0.001, Pgroup 4 vs group 2 < 0.001) and TC (Pgroup 4 vsgroup 1 < 0.001, Pgroup 4 vs group 2 = 0.018), whereas the increased percentage of family history of diabetes (Pgroup 4 vsgroup 1 < 0.001, Pgroup 4 vs group 2 < 0.001). With prolonged diabetic status, there was a significantly decreasing trend in the proportion of patients who used diet and exercise alone to control blood glucose (28.70%, 16.96%, 10.06%, 3.92%, P < 0.001). Compared to group 1, the level of HbA1c was significantly higher in group 4 (7.40% vs 7.10%, P = 0.015), but was significantly lower in group 2 (6.70% vs 7.10%, P < 0.001) and group 3 (7.00% vs 7.10%, P = 0.002).
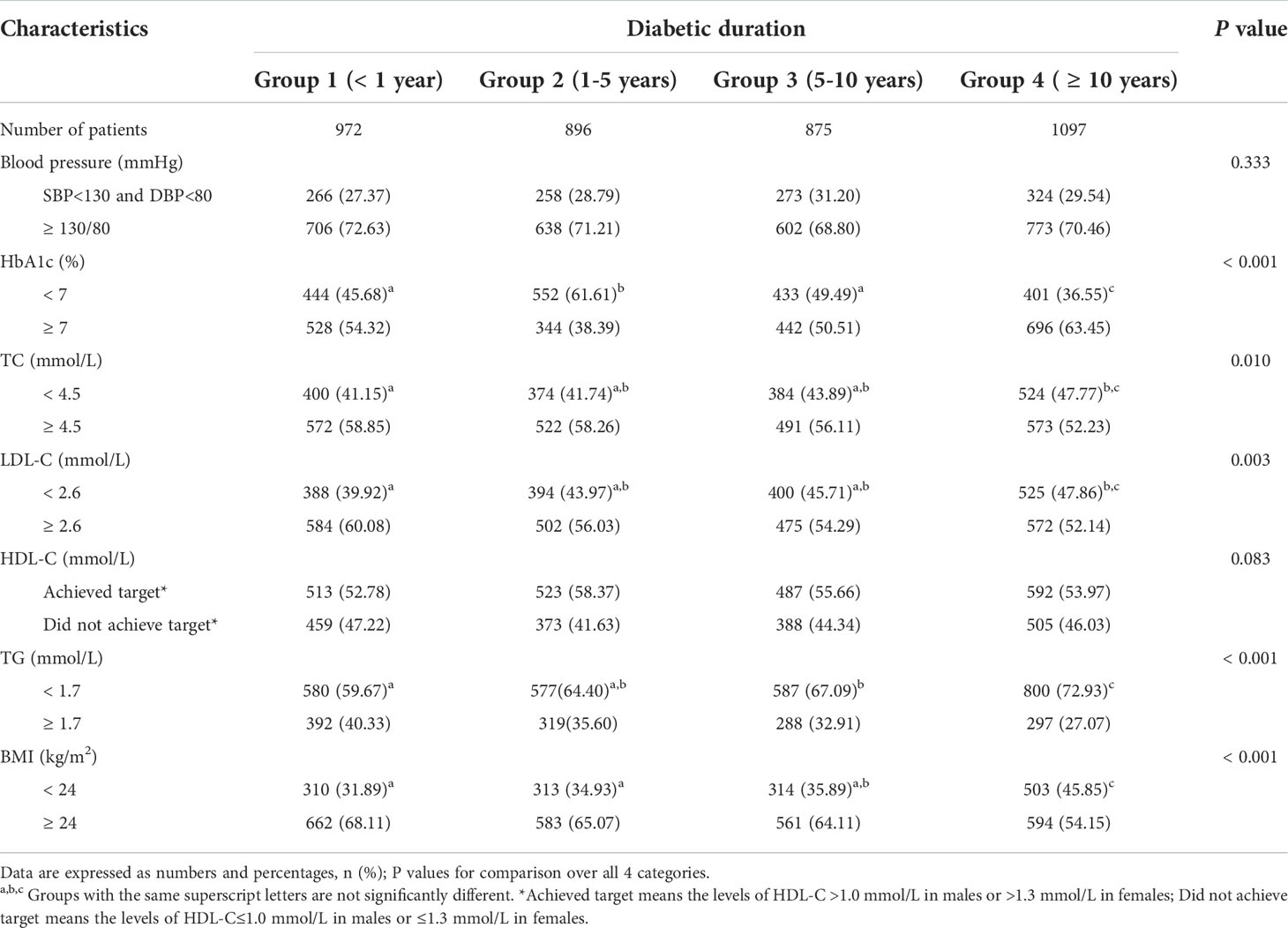
Control rates of T2DM targets among elderly patients with different durations
The control rates of T2DM targets in elderly patients with T2DM between different groups are shown in Table 2. Compared to group 1, the control rate of HbA1c was higher in group 2 (61.61% vs 45.86%, P < 0.001), whereas the rate was significantly lower in group 4 (36.55% vs 45.86%, P < 0.001). Group 4 had a significantly higher control rate of TC when compared with groups 1 (47.77% vs 41.15%, P = 0.018). The similar results were observed for the control rates of LDL-C (47.86% vs 39.92%, P = 0.002). Patients of group 4 were more likely to be higher control rate of TG and BMI when compared with other groups (all P < 0.05). Additionally, no significant differences in the control rates of blood pressure and HDL-C were found across the groups with various durations of diabetes (all P > 0.05).
As shown in Table 3, after adjusting for age, sex, education, BMI, smoking and family history of diabetes (model 3), T2DM patients in group 2 had significantly increased OR for achieving the control target for HbA1c (ORHbA1c = 1.92, 95% CI = 1.59-2.31, P < 0.001), while elderly T2DM patients in group 4 showed significantly decreased OR for achieving the control target for HbA1c (ORHbA1c = 0.65, 95% CI = 0.54-0.78, P < 0.001). The significantly increased ORs for achieving the control targets for TC (ORTC = 1.36, 95% CI =1.14-1.63, P < 0.001), LDL-C (ORLDL-C = 1.39, 95% CI =1.17-1.66, P < 0.001) and BMI (ORBMI = 1.82, 95% CI =1.52-2.18, P < 0.001) were observed in group 4. Interestingly, we observed the gradually increased ORs for achieving the control targets for TC with the prolonged duration of diabetes (ORgroup 2 = 1.75, 95% CI =1.45-2.12; ORgroup 3 = 1.38, 95% CI =1.13-1.68; ORgroup 4 = 1.76, 95% CI =1.46-2.14; P < 0.001) in model 3.
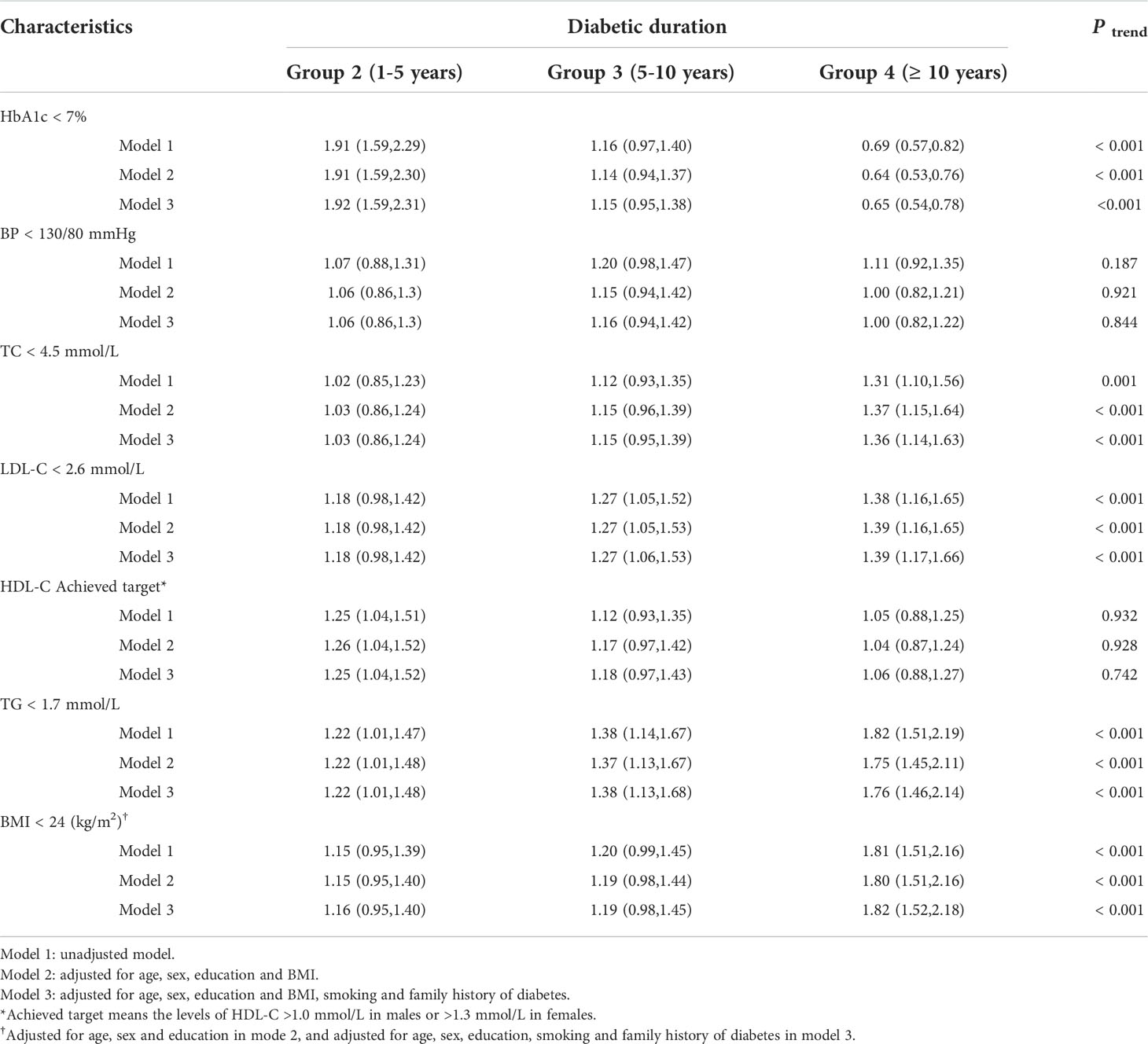
Table 3 Odds ratios (95% CI) for achieved comprehensive control targets by different diabetic duration groups among elderly patients with T2DM (Ref. < 1 year).
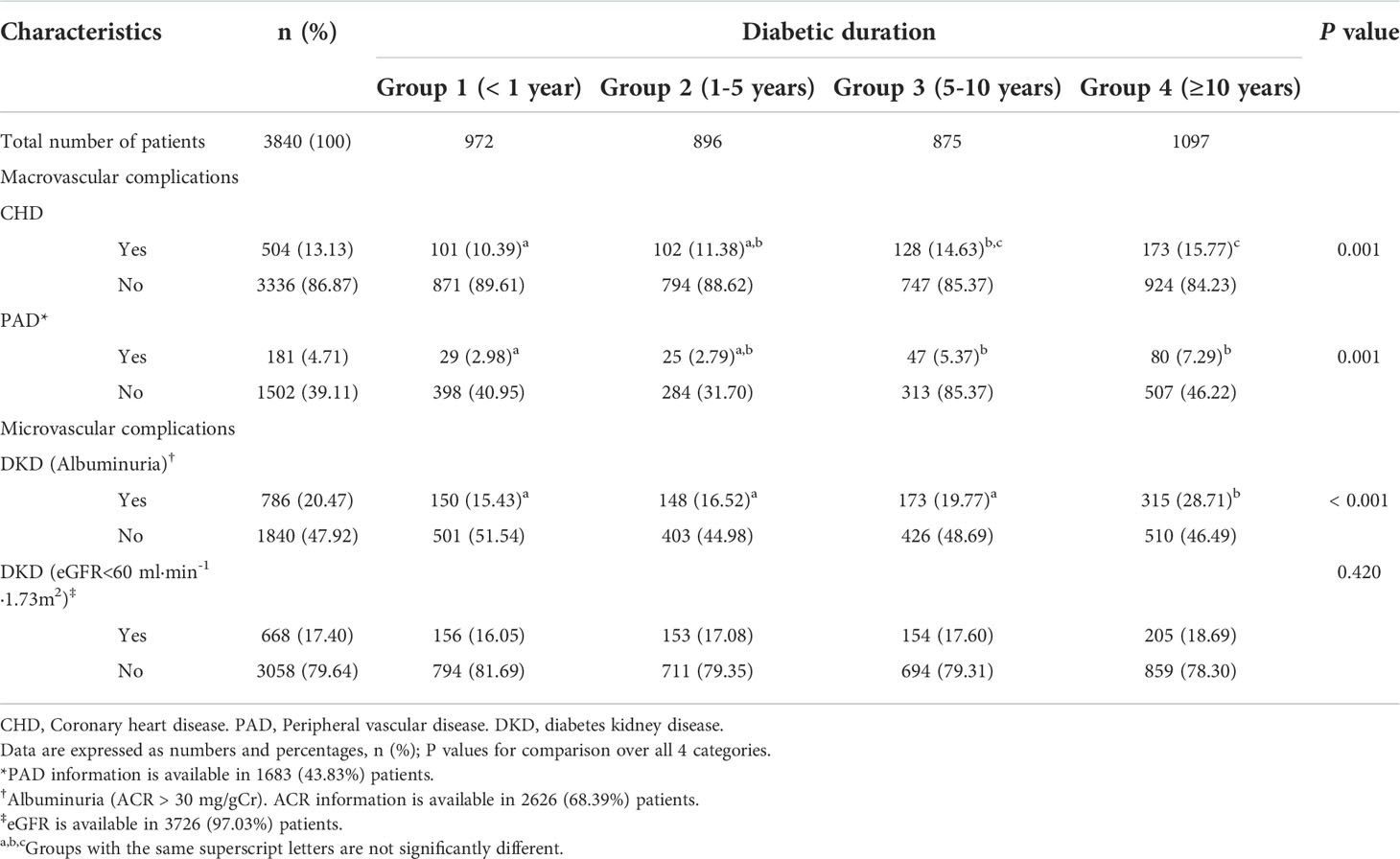
Macrovascular and microvascular complications of diabetes among the groups
The prevalence of diabetic macrovascular and microvascular complications among the groups are presented in Table 4. Notably, there are 2157 (56.18%) patients with missing PAD data, 1214 (31.61%) with missing albuminuria, and 114 (2.97%) with missing eGFR. Between the four groups, there was no significant difference in the percentage of patients with eGFR<60 ml·min-1 ·1.73m2 (P = 0.420). Compared to group1, group 4 had the higher percentage of patients with CHD, PAD and albuminuria (all P < 0.05). As shown in Table 5, after adjusting for potential confounders, we observed elderly T2DM patients in groups 3 and 4 had significantly increased ORs for CHD (ORgroup 3 = 1.43, 95% CI =1.07-1.89; ORgroup 4 = 1.56, 95% CI =1.19-2.04; P trend< 0.001) and for PAD (ORgroup 3 = 1.82, 95% CI =1.10-3.01; ORgroup 4 = 1.60, 95% CI =1.00-2.55; P trend= 0.022) in model 3. Patients in group 4 had significantly increased ORs for albuminuria (OR albuminuria = 1.96, 95% CI =1.55-2.48, P trend < 0.001; OR eGFR = 1.36, 95% CI =1.05-1.75, P trend =0.030).
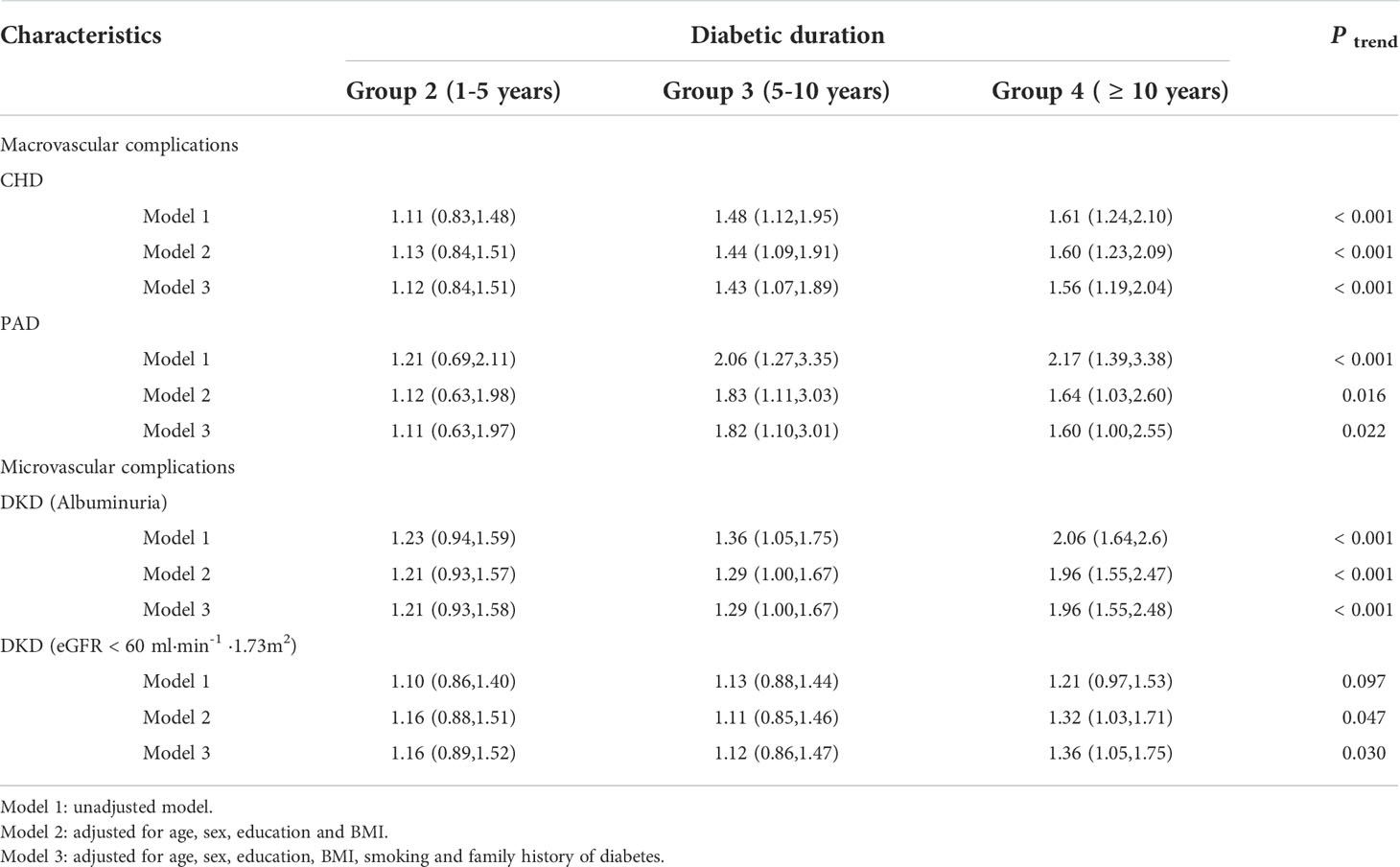
Table 5 Odds ratios (95% CI) for macrovascular and microvascular complications by different diabetic duration groups among elderly patients with T2DM (Ref. < 1 year).
Discussion
In the current study, we evaluated the comprehensive control of T2DM and diabetic complications in elderly patients stratified by different durations of diabetes. Elderly T2DM patients with a duration of diabetes of ≥ 10 years were more likely to achieve the comprehensive control targets for TC, LDL-C and TG, while elderly T2DM patients with a duration of diabetes of 1~5 years were more likely to achieve the HbA1c control target than elderly T2DM patients with a duration of diabetes of < 1 year. In elderly T2DM patients with a duration of diabetes of 5~10 years or ≥ 10 years, the duration of diabetes was independently associated with diabetic macrovascular complications (CHD and PAD). In addition, in patients with a duration of diabetes of ≥ 10 years, the duration of diabetes was independently associated with the risk of DKD.
HbA1c is typically used as the gold standard for evaluating glycaemic control and is a clinical indicator for predicting diabetic complications (4). In addition, HbA1c < 7% is the standard for good glycaemic control in most adults with T2DM that is recommended by most guidelines (4, 6). Previous studies have shown that the ORs of poor glycaemic control increase with diabetes duration in T2DM (14, 15). Interestingly, in the current study, elderly T2DM patients with a duration of diabetes of 1~5 years were more likely to achieve the HbA1c control target than those who had a duration of diabetes less than 1 year, and the control target rate of HbA1c gradually decreased with the extension of the duration. The reasons for this finding are still unclear but may be caused by differences in study design, the deterioration of islet function with diabetes progression (16), or the clinical criteria for glycaemic control (17).
Dyslipidaemia is one of the most important risk factors for CHD, and optimal lipid control can improve cardiovascular outcomes (18). Our study found that the higher control rates for TC, LDL-C, TG and BMI were observed in elderly T2DM patients with a duration of diabetes of ≥ 10 years than that in patients who had a duration of diabetes less than 1 year. A possible reason is that since the similar prevalence of CHD and PAD was observed in patients with a duration of diabetes of ≥ 10 years, elderly patients with T2DM may pay more prone to it. Another reason is that the elderly patients with long duration may use lipid-lowering or antiplatelet agents to relieve symptoms. Further studies with more detail information should be performed to explore the underlying reasons.
Previous cohort studies have reported that the duration of diabetes is associated with the risk of developing diabetes-related complications in aged T2DM patients (19, 20). One study in the USA showed that the prevalence of CHD, PAD and cerebrovascular disease was significantly higher in elderly T2DM patients (aged ≥ 60 years) with a duration of diabetes ≥ 10 years than in those with a shorter duration (19). Furthermore, another study in Australia reported that the incidences of myocardial infarction and stroke-related death increased along with an increase in the duration of diabetes in 1433 aged male patients with diabetes (aged ≥ 65 years) (20). Our study also found that elderly T2DM patients with a duration of diabetes of 5~10 years or ≥ 10 years were more likely to develop diabetic macrovascular complications (CHD and PAD) than those with a duration of diabetes of <1 year, which was consistent with the abovementioned studies. Moreover, the present study also suggested that the duration of diabetes was significantly associated with microvascular complications (albuminuria), which is in accordance with a previous study (21).
There were several limitations in our study. First, there is missing data on outcomes of interest including PAD and DKD, and our study was a cross-sectional and single-center study. Future large and longitudinal studies with these outcomes are needed to confirm the associations. Second, the preference of doctors on medication regiment and drug choice might influence the analytic data on characteristics of the elderly T2DM patients based on diabetes duration. Data on the detail medication and medication adherence of patients should be considered into further studies.
In summary, elderly T2DM patients with a duration of diabetes of 1~5 years were more likely to achieve the HbA1c control target, while patients with a duration of diabetes of ≥ 10 years were more likely to achieve the comprehensive control targets for the lipid profile. In addition, the duration of diabetes was independently associated with diabetic macrovascular complications (CHD and PAD) in elderly T2DM patients with a duration of diabetes of 5~10 years or ≥ 10 years and was significantly associated with DKD in patients a duration of diabetes of with ≥ 10 years.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the corresponding author, without undue reservation.
Author contributions
WT and YY conceived and design the research. YY and KX analyzed the data. QL, HX, DW, LD, CH, SS, and KW collected the data. YY and KX wrote and revised the initial manuscript. WT supervised the whole study and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81770773), Natural Science Foundation of Jiangsu Province (BK20211375), the Foundation of Jiangsu Province Health Bureau (BJ18008), and Cohort study of elderly type 2 diabetes from Nanjing Medical University (NMUC2020041).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sinclair A, Saeedi P, Kaundal A, Karuranga S, Malanda B, Williams R. Diabetes and global ageing among 65-99-year-old adults: Findings from the international diabetes federation diabetes atlas, 9(th) edition. Diabetes Res Clin Pract (2020) 162:108078. doi: 10.1016/j.diabres.2020.108078
2. Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA (2017) 317:2515–23. doi: 10.1001/jama.2017.7596
3. Wu H, Eggleston KN, Zhong J, Hu R, Wang C, Xie K, et al. Direct medical cost of diabetes in rural China using electronic insurance claims data and diabetes management data. J Diabetes Invest (2019) 10:531–8. doi: 10.1111/jdi.12897
4. American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2020. Diabetes Care (2020) 43:S14–31. doi: 10.2337/dc20-S002
5. Chen R, Ji L, Chen L, Chen L, Cai D, Feng B, et al. Glycemic control rate of T2DM outpatients in China: a multi-center survey. Med Sci Monit Int Med J Exp Clin Res (2015) 21:1440–6. doi: 10.12659/MSM.892246
6. Chinese Diabetes S. Guideline for the prevention and treatment of type 2 diabetes mellitus in China(2020 edition). Chin J Endocrinol Metab (2021) 37:311–98. doi: 10.3760/cma.j.cn115791-20210221-00095
7. Dailey G. Early and intensive therapy for management of hyperglycemia and cardiovascular risk factors in patients with type 2 diabetes. Clin Ther (2011) 33:665–78. doi: 10.1016/j.clinthera.2011.04.025
8. Yu Y, Xie K, Lou Q, Xia H, Wu D, Dai L, et al. The achievement of comprehensive control targets among type 2 diabetes mellitus patients of different ages. Aging (2020) 12:14066–79. doi: 10.18632/aging.103358
9. Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes (2008) 26:77–82. doi: 10.2337/diaclin.26.2.77
10. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic Med J Br Diabetic Assoc (1998) 15:539–53. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
11. Matsushita K, Mahmoodi BK, Woodward M, Emberson JR, Jafar TH, Jee SH, et al. Comparison of risk prediction using the CKD-EPI equation and the MDRD study equation for estimated glomerular filtration rate. JAMA (2012) 307:1941–51. doi: 10.1001/jama.2012.3954
12. K.D.I.G. Outcomes, C.W.G.J.K. Int. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. (2013) 3:1–150. doi: 10.1038/kisup.2012.77
13. Andrassy KM. Comments on 'KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease'. Kidney Int (2013) 84:622–3. doi: 10.1038/ki.2013.243
14. Li J, Chattopadhyay K, Xu M, Chen Y, Hu F, Chu J, et al. Glycaemic control in type 2 diabetes patients and its predictors: a retrospective database study at a tertiary care diabetes centre in ningbo, China. BMJ Open (2018) 8:e019697. doi: 10.1136/bmjopen-2017-019697
15. Fiseha T, Alemayehu E, Kassahun W, Adamu A, Gebreweld A. Factors associated with glycemic control among diabetic adult out-patients in northeast Ethiopia. BMC Res Notes (2018) 11:316. doi: 10.1186/s13104-018-3423-5
16. Hayashino Y, Izumi K, Okamura S, Nishimura R, Origasa H, Tajima N. Duration of diabetes and types of diabetes therapy in Japanese patients with type 2 diabetes: The Japan diabetes complication and its prevention prospective study 3 (JDCP study 3). J Diabetes Invest (2017) 8:243–9. doi: 10.1111/jdi.12550
17. Reach G, Pechtner V, Gentilella R, Corcos A, Ceriello A. Clinical inertia and its impact on treatment intensification in people with type 2 diabetes mellitus. Diabetes Metab (2017) 43:501–11. doi: 10.1016/j.diabet.2017.06.003
18. American Diabetes Association. Cardiovascular disease and risk management: Standards of medical care in diabetes-2020. Diabetes Care (2020) 43(Suppl. 1):S111–34. doi: 10.2337/dc20-ad08
19. Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Internal Med (2014) 174:251–8. doi: 10.1001/jamainternmed.2013.12956
20. Yeap BB, McCaul KA, Flicker L, Hankey GJ, Almeida OP, Golledge J, et al. Diabetes, myocardial infarction and stroke are distinct and duration-dependent predictors of subsequent cardiovascular events and all-cause mortality in older men. J Clin Endocrinol Metab (2015) 100:1038–47. doi: 10.1210/jc.2014-3339
Keywords: clinical characteristics, elderly patients, type 2 diabetes mellitus, duration of diabetes, control targets
Citation: Yu Y, Xie K, Lou Q, Xia H, Wu D, Dai L, Hu C, Shan S, Wang K and Tang W (2022) The clinical characteristics of Chinese elderly patients with different durations of type 2 diabetes mellitus. Front. Endocrinol. 13:904347. doi: 10.3389/fendo.2022.904347
Received: 25 March 2022; Accepted: 05 July 2022;
Published: 29 July 2022.
Edited by:
Helena Cristina Barbosa, State University of Campinas, BrazilReviewed by:
Lingou Li, First People’s Hospital of Chongqing Liangjiang New District, ChinaByung-Wan Lee, Yonsei University, South Korea
Copyright © 2022 Yu, Xie, Lou, Xia, Wu, Dai, Hu, Shan, Wang and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Tang, drtangwei@njmu.edu.cn
†These authors have contributed equally to this work
 Yun Yu1†
Yun Yu1† Wei Tang
Wei Tang